Choosing the Right Treatment for Vaginal Atrophy: Renovalase vs. MonaLisa Touch
Are you experiencing vaginal dryness, painful intercourse, or general discomfort? You’re not alone. These symptoms, often associated with menopause, can significantly impact your quality of life. However, it’s essential to understand your treatment options thoroughly to find the solution that best fits your needs. In this article, we’ll compare two popular treatments for vaginal atrophy: Renovalase and Mona Lisa Treatment (Mona Lisa Touch Treatment).
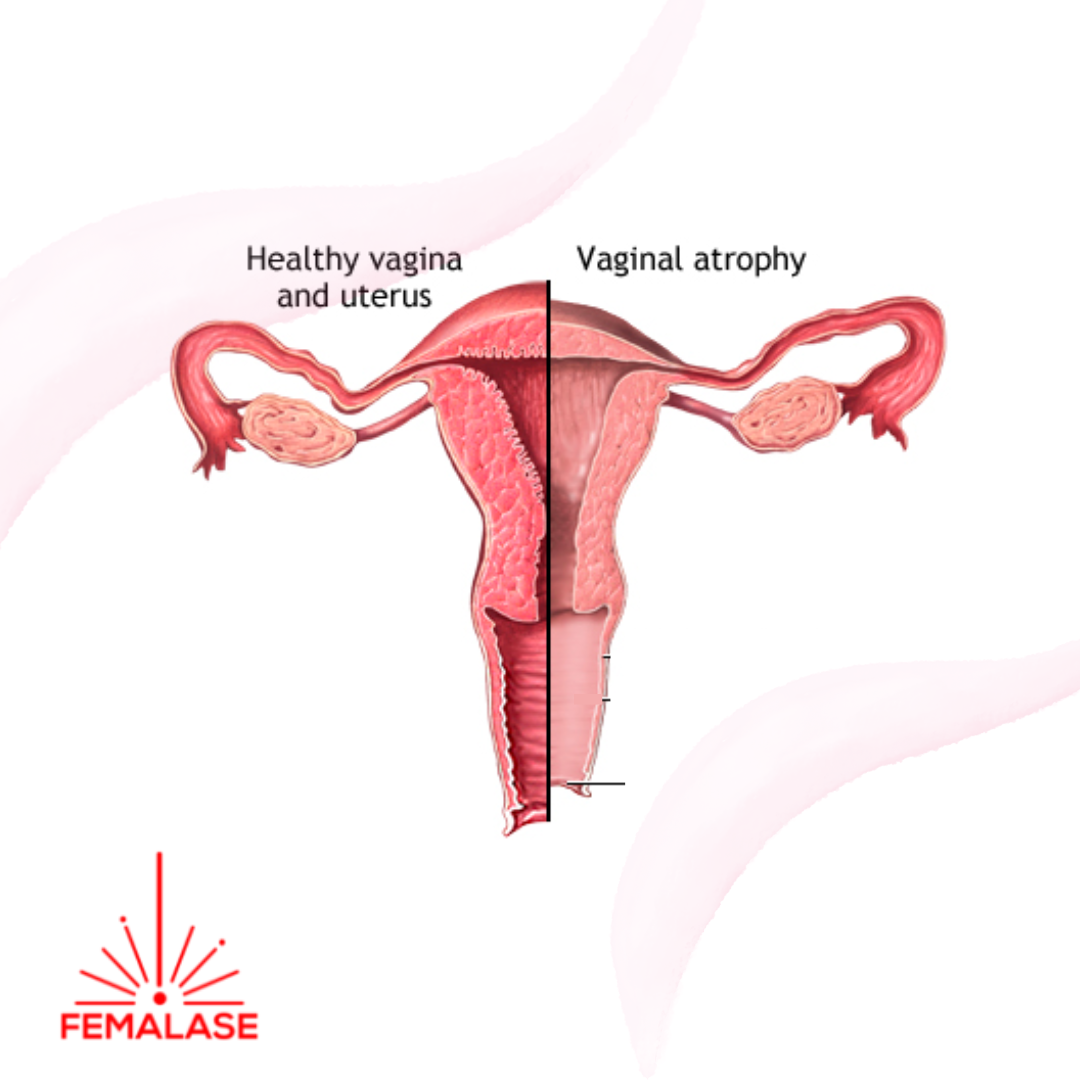
Understanding Vaginal Atrophy
Vaginal atrophy is a common condition caused by decreased estrogen levels, particularly during menopause. This hormonal shift leads to thinning and degeneration of the vaginal mucosa, resulting in symptoms like dryness, irritation, and pain during intercourse. Addressing vaginal atrophy is crucial for restoring comfort and improving overall well-being.
The Mona Lisa Touch Treatment Approach
Mona Lisa Touch Treatment is a CO2 laser therapy designed to address vaginal atrophy by stimulating collagen production and restoring vaginal tissue health. This treatment aims to prevent and resolve estrogen drops in the vaginal tissue, offering a non-surgical and non-pharmacological solution for women experiencing menopausal symptoms.
Key Benefits of MonaLisa Touch®:
Collagen Regeneration: By reactivating collagen production, MonaLisa Touch® promotes tissue regeneration, leading to improved vaginal health and elasticity. The treatment lasts usually a few minuets and does not cause discomfort. Patients may experience improved hydration, thicker epithelium, and restored vaginal pH, enhancing overall quality of life and personal relationships.
Renovalase, on the other hand, is a cutting-edge non-invasive laser therapy specifically developed for the symptoms of vaginal atrophy. Utilizing non-ablative photothermal treatment, Renovalase targets the vaginal canal to restore the vaginal mucosa to a premenopausal state, offering efficient and quick results.
Key Benefits of Renovalase:
Efficient Treatment: Clinical studies demonstrate the effectiveness of Renovalase in addressing vaginal atrophy symptoms, providing rapid relief and restoration.
Non-Ablative Technology: Unlike previous laser treatments, Renovalase employs Er:Yag laser technology, minimizing risks such as scarring and pain associated with previous methods.
Comprehensive Restoration: By treating the problem at its source, Renovalase offers comprehensive vaginal rejuvenation, addressing issues like dryness and discomfort effectively.
Choosing the Right Treatment for You
When deciding between MonaLisa Touch® and Renovalase, it’s essential to consider your individual needs and preferences. While both treatments offer significant benefits for vaginal health, Renovalase stands out for its efficiency, safety, and comprehensive restoration.
If you’re seeking a solution that provides rapid results and minimizes discomfort, Renovalase may be the ideal choice for you. Contact us today to learn more about Renovalase and schedule your consultation. Don’t let vaginal atrophy impact your quality of life – take the first step towards renewal and rejuvenation with Renovalase. Conact us today for guidance.